Centene Corporation is the largest provider of “Obamacare,” Medicare and Medicaid in the country. It operates under many different names, depending on the setting, the state and the function of the product it represents. Some common names you’ll encounter when doing addiction treatment billing are: Ambetter, HealthNet, Fidelis Care, Ascension Complete, Centurion, Celtic, Qualchoice, and Meridian. Many of these brand names are further customized depending on the state, like “Ambetter from Peach State Health,” which refers to Georgia’s Marketplace health care program.
We’ve written elsewhere about Centene and how to appeal an addiction treatment claim denial, but today we’ll discuss what the actual rates of denial are with Centene when it comes to behavioral health. We’ll also look at what levels of care are most likely to be denied at Centene and why.
Centene Has a Long History of Denying Behavioral Health Claims in All of its Various Brand Names
If you’re seeing a lot of addiction treatment claims denials from Centene or one of its companies, you’re in good company. Centene has a terrible denial rate, especially when it comes to addiction treatment. While the company makes a good show of promoting parity and health care equity for all patients, even those with behavioral health conditions, its coverage decisions demonstrate the opposite.
Centene Corporation's CEO, Michael Neidorff earned $20.6 million dollars in a single year. He also oversaw an organization that denied behavioral healthcare claims at rates as high as double the national average.
Many of Centene’s businesses have been on the receiving end of lawsuits regarding what some providers see as a lack of transparency in behavioral health care coverage. In a California case, HealthNet, Inc, a subsidiary of Centene Corporation, received several warnings about not violating state and federal law by skipping out on justly due compensation for behavioral health care workers. FierceHealthcare has seen similar legal action.
Centene Uses Several Techniques for Maximizing its Denial Rates for Addiction Treatment Claims
Centene doesn’t just use one technique to deny addiction treatment and behavioral health claims. This payer has an arsenal of tools it uses to ensure that patients with SUD don’t become a financial liability to the company.
Here’s just a few of the methods Centene Corporation companies use to protect their bottom line and withhold healthcare from SUD patients:
“Robo-signing” medical necessity denials
Demanding proof of residency from would-be addiction treatment patients
Requiring proof from addiction treatment centers that patients have not received incentives to sign up for rehab
Extensive and elaborate prior authorization requirements
Referral requirements
Denials based on data entry errors
Denials based on trivial paperwork mistakes
Pushing the lowest level of care possible
Restricting addiction treatment care to PCP visits
Offering outpatient instead of residential, intensive inpatient or partial hospitalization
Centene is Among the One in Five Insurers Who Deny More Than 30% of In-Network Behavioral Health Claims
The average marketplace payer issues denials to 18% of in-network claims, whether they’re general claims or behavioral health-related claims. Centene Corporation businesses, on the other hand, frequently issue denials to 30% or more of in-network claims for all types of healthcare, including behavioral health claims.
At Centene, Behavioral Health Claims are Disproportionately Denied Based on Lack of “Medical Necessity”
When you look at all payers together as one, you find that, on average, just 2% of denied claims are denied on the grounds of medical necessity. The vast majority of insurance claim denials are based on clerical errors, while exclusions and prior authorization issues make up the bulk of the remainder. In other words, it’s quite rare for a payer to use medical necessity as a justification for denying a claim.
However, it’s not at all rare for payers to use medical necessity as a basis for denying behavioral health claims, and this state of affairs is no different when it comes to Centene Corporation and its various subsidiaries. In fact, one in five claims denied on the basis of medical necessity are behavioral health claims.
This means that payers like Centene promise to cover behavioral healthcare on paper, but in actuality, they place heavy restrictions on accessing lifesaving care for SUD patients. They’ll provide coverage - but only if it’s “medically necessary.” Conveniently, addiction treatment is deemed not medically necessary more frequently than other types of healthcare interventions.
Centene Corporation Denial Rates for Addiction Treatment By the Numbers
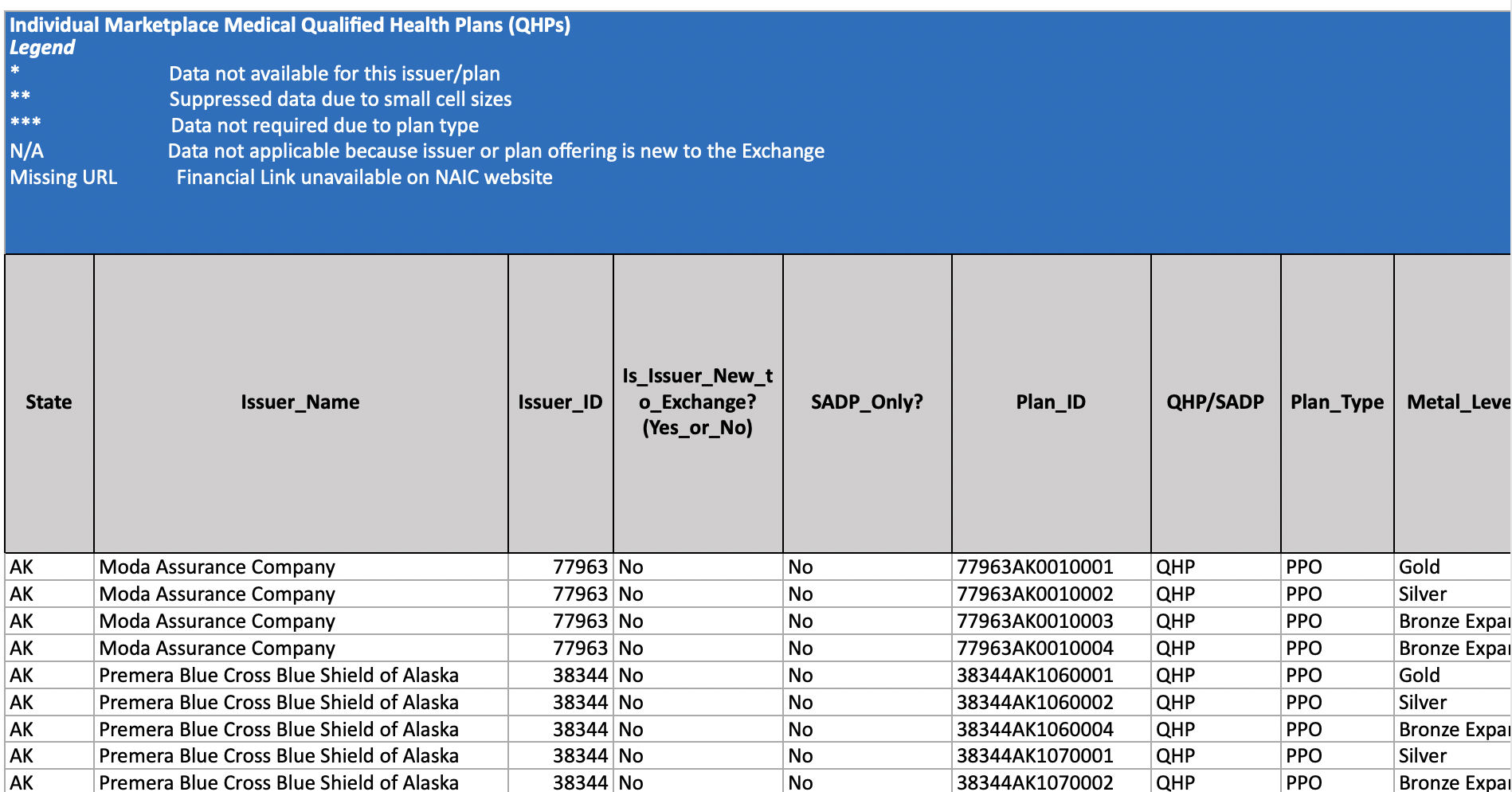
Because Centene Corporation does business under so many different names, it is difficult to generalize about a single “denial rate” for the company - let alone a single “denial rate” for behavioral health claims at Centene. However, a recent report released by the Kaiser Foundation sheds some light on the situation.
The report, which lists claims, denials and appeals in ACA Marketplace Plans in 2020, lists the total number of claims, the total number of denials and the total number of medical necessity denials that are NOT related to behavioral healthcare for each of Centene’s various companies. Furthermore, the report breaks out denial information by plan, for example, a Bronze plan will have a single data set and a Gold plan will have another. The information provided is granular but when aggregated together it gives a decent picture of Centene Corporation's track record for behavioral health denials.
For example, Celtic patients in Arkansas enrolled in the Silver plan see their healthcare claims denied 34% of the time, with 58374 denials total in a single year. Of those denials, an unknown portion were based on medical necessity. Of that group, only 54 claims were NOT related to medical necessity and behavioral health. In other words, the vast majority of medical necessity denials at Celtic are behavioral health denial.
You can see the whole report here under “Benefits and Cost Sharing PUF.”
Tired of Searching for Insight into How to Manage Your Partnership with Centene Corporation? We Can Help.
Behave Health is committed to making it easier - and more profitable - to operate evidence-based, results-focused addiction treatment centers.
Get your free trial started today and see why more addiction treatment centers prefer Behave Health.
Need help with certification? Behave Health can also help direct you to the right resources for help with Licensing or Accreditation by either The Joint Commission or CARF. Mention to your product specialist that you’re interested in this service after you start your free trial!